By Sarah Paris
Freely accessible for the first time, the virtual Precision Medicine World Conference on COVID-19 (PMWC) drew more than four times its normal attendance this January, with over 10,000 registrants from 101 countries. As in previous years, the three-day conference was co-hosted by a UCSF team under the leadership of Keith Yamamoto, PhD, director of UCSF Precision Medicine and vice chancellor for Science Policy and Strategy. Eleven UCSF faculty discussed their work, representing the largest contingent from any institution.
BREAKTHROUGHS FACE VALLEY OF DEATH
In his opening remarks, Yamamoto stressed how the COVID-19 pandemic served both as a disrupter and a catalyst for innovation and unprecedented collaboration, “a glimpse of what open science could look like.”
“It is clear that covid has been an effective catalyst for change, some of it positive, and we hope these positive changes can be maintained,” he said. However, the impact on non-covid research has been “devastating,” said Yamamoto, noting his hope that the new U.S. administration will recognize and ameliorate the setback.
Among the scientists whorapidly pivoted to COVID-19-related research was a team led by Peter Walter, PhD. They launched an unprecedented collaboration with other teams and created AeroNabs, tiny, heat-stable antibodies with coronavirus-neutralizing activity after aerosol delivery. In the opening session of the conference, focused on “COVID-19 as Disrupter of Biomedical Research and Healthcare,” Walter contrasted the “heartwarming experience of seeing scientists jell and bring their research together,” with his “incredible frustration” when the promising result of their collaboration became trapped in the so-called “valley of death” – a term describing the challenge of finding an industry partner who will conduct the clinical trials needed for a new therapeutic to receive FDA approval.
What the landscape lacks, according to Walter, is a bridge that spans the gap and connects the two sides; a role for which the government might be best suited.

AeroNabs co-creator, Aashish Manglik, MD, PhD, outlined the science behind this remarkable discovery on day two of PMWC. The session on developing new therapeutics also included his colleague Danielle Swaney, PhD, who related her team’s powerful strategy to discover every human protein that interacts with any SARS-CoV-2 protein as an approach to repurpose existing drugs that interact with those host proteins as potential antivirals.
FRESH ENERGY HITS OUTDATED SYSTEMS
The theme of COVID-19 as a driver for change echoed throughout the conference. In a panel on molecular testing, Joe DeRisi, PhD, recalled the effort to turn his lab at the Chan Zuckerberg Biohub into a highly productive testing facility, ultimately providing genomic sequencing for public health departments in the Bay Area and beyond. He praised the efforts of hundreds of UCSF graduate students and postdocs who worked long shifts to keep the lab going. But he also expressed his frustration with fractured systems, fragmented data, and infrastructure so outdated that “we oftentimes had to rely on Fax machines to communicate.”
In a related panel session on the testing ecosystem, Charles Chiu, MD, PhD, similarly pointed out the weaknesses in a system ill prepared for the pandemic, including breaks in the supply chain. “At various points we lacked swabs, ran out of tips … even dry ice for storage.”
“We need to rebuild our public health infrastructure,” Chiu said. “It’s decimated, and it shows, and it’s embarrassing.” Like other speakers at the conference, Chiu and DeRisi strongly advocated for a unified national response to curb the pandemic, and to prevent or better prepare against future threats.
COVID IS NOT THE ONLY THING THAT KILLS PEOPLE
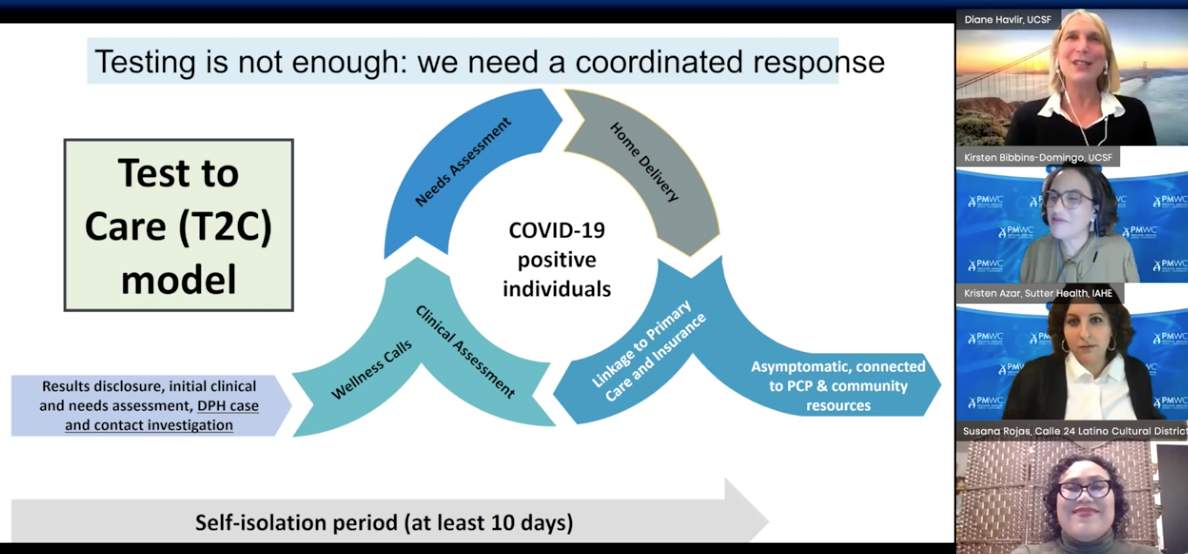
The impact of COVID-19 on mental health and cancer care, and the widening of health disparities, were further topics brought to the forefront of the conference. UCSF Department of Epidemiology and Biostatistics Chair Kirsten Bibbins-Domingo, MD, PhD, and UCSF Professor of Medicine Diane Havlir, MD, discussed how the Latinx community in the Bay Area continues to be hardest hit, and how UCSF has responded with locally targeted testing, in partnership with community organizations and leaders such as Susanna Rojas, director of Calle 24. Havlir underscored the need for a low-barrier, rapid “test and respond”, community-facing approach that includes social interventions, such as a wage-replacement program (“Right to Recover”) to enable infected workers to stay at home.
The pandemic also required a massive rerouting of patients requiring regular care, from in-person to remote visits enabled by videoconferencing technologies. Shifting to this telehealth model for routine visits prompted a rethinking of systems and habits. For patients living hours away from the clinic, the new model has shown benefits, though with the caveat that telehealth is by no means accessible to all. Pointing to the silver lining, UCSF Cancer Center’s Pelin Cinar, MD, noted that “we have shown ourselves adaptable. We were able to implement interventions within days.”
Her colleague Laura Esserman, MD, a long-time advocate for personalized treatment of cancer patients and leader of the I-SPY Trials (including the I-SPY COVID trial) called for a renewed effort to identify and focus on high-risk patients and avoid over-treatment of those at low risk. The pandemic, she argued, is an impetus to break down inefficient systems and gain the ability to conduct speedier clinical trials to produce the data needed to validate patient-centered treatment plans.
“That sense of urgency to solve problems should not go away. Covid is not the only thing that kills people. Our patients don’t have ten years for us to get our act together,” Esserman said.

PRECISION MENTAL HEALTH
Though it should be obvious that precision medicine includes the whole person, mental health is frequently left out of the discussion. COVID-19, however, led to a “phenomenal wake-up call,” according to Elissa Epel, PhD. A panel session on the impact of the pandemic on stress and depression pointed out some disturbing statistics, including a rise in depression among young adults, with 1 in 4 reportedly considering suicide during this past year.
The good news, Epel pointed out, is that precision medicine has revealed novel targeted interventions for patients with severe familial depression and a corresponding genetic or neuroactivity profile. However, the pandemic has exacerbated the social pressures that create stress-induced mild or moderate depression. Not surprisingly, black, indigenous, and people of color suffer disproportionally. While medication may be helpful for some people, integrative methods, including nutrition, mind-body exercises, and especially social support may be more effective. “If we don’t hit the big stressors like food insecurity and racism, we will never eliminate toxic stress,” said Epel.
Julianne McCall, PhD, co-director of the California Initiative to Advance Precision Medicine, noted the fragmentation of care that puts mental health into a separate category, similar to dentistry, which causes further societal inequities and data silos that inhibit the connections vital to precision medicine. She highlighted that the Governor’s budget proposal includes plans to streamline care for Medi-Cal patients and build upon an existing health information exchange to expand the use of data to benefit of patients.
FAUCI, TOPOL, WOODCOCK
Further highlights of the conference included a session on computational strategies with Eric Topol, MD; a discussion of regulatory issues with FDA acting commissioner Janet Woodcock, MD; and a conversation with Anthony Fauci, MD, who received the PMWC Luminary award.
The conference made clear that extending collaborations across disciplines and an open science approach has resulted in unprecedented innovation during this challenging year. It also amplified the need to overhaul and align public health systems and data exchanges to meet the present and future health threats.
