 What are some common misconceptions about precision medicine? What is a knowledge network, and how is it boosting research and clinical practice at UCSF? Who benefits?
What are some common misconceptions about precision medicine? What is a knowledge network, and how is it boosting research and clinical practice at UCSF? Who benefits?
In this interview, Keith Yamamoto, PhD, Director of UCSF Precision Medicine, explains why UCSF is considered a leader in the field and describes the "machine" created to fuel new insights and innovation.
By Sarah Paris
Q1. Five years ago, Chancellor Hawgood named precision medicine as one of his four priorities. What progress has been made to create this new “research matrix” and promote a precision medicine approach across disciplines?
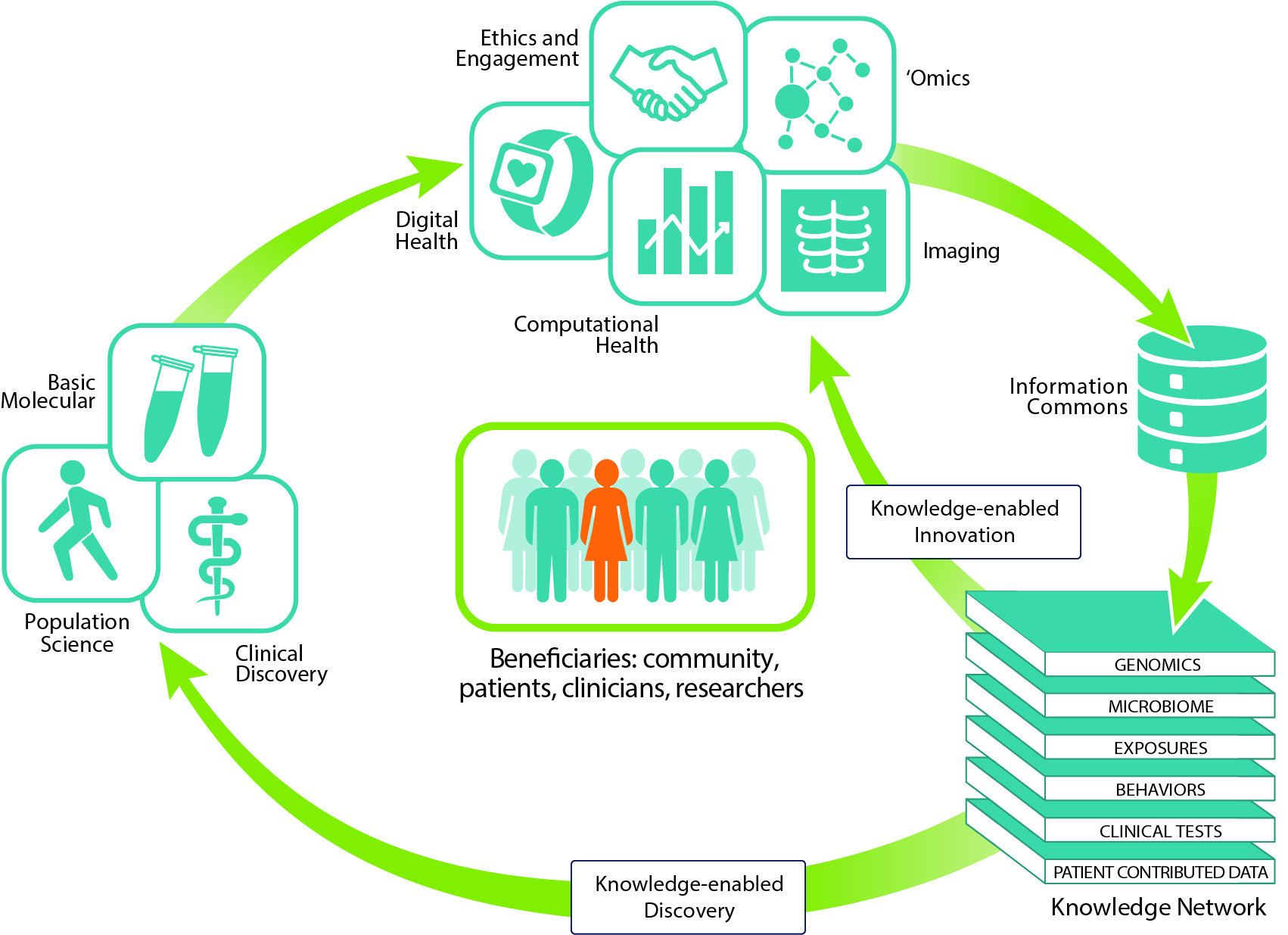
KY: Precision medicine engages high-powered computational tools to integrate and advance biomedical research, health and healthcare. At UCSF, we have created and are progressively expanding a dynamic “machine” or matrix that is keeping this process in motion.
The many types of data generated by this matrix populate an “information commons” where the data are standardized for use through machine learning and AI algorithms. This process reveals patterns and connections between the data layers of the knowledge network. These new insights in turn fuel iterative cycles of new hypotheses for basic scientists or potential new pathways for treatments, prevention, or even cures to be investigated by clinical and population scientists.
Q.2 Have other institutions created similar, large-scale approaches to precision medicine?
KY: I am not aware of another institution that is taking such a full spectrum approach. As someone who talks with many people outside of UCSF, I can say that in Congress, in federal agencies, and in various foundations and non-profits, we are widely viewed as a leader, if not the leader, in precision medicine.
As one example, we were tapped by NSF’s Convergence Accelerator program to head the development of a large-scale biomedical knowledge network in collaboration with Google, Lawrence Livermore National Laboratory, and Institute for Systems Biology. And next week, 31 UCSF researchers will be presenting at Precision Medicine World Conference, by far the largest contingent from any institution.
Q3. What is your role in implementing Precision Medicine at UCSF and nationally?
My outward-facing role as vice chancellor for science policy and strategy includes advocating for precision medicine as a new imperative in science and bringing visibility to UCSF’s pioneering activities in that realm, which can be adopted, adapted, shared or improved upon by others. In that context, I also help to create partnerships and collaborations with other institutions and organizations.

Internally, my role at UCSF as director of precision medicine is to identify opportunities and needs within the precision medicine model environment we are creating. This involves working with the leaders of each of the elements, as well as developing topical programs in areas such as cancer, neuroscience/neurology, women, children, public health, immunology, and microbiomes. My job is to establish these groups such that they realize the synergies that emerge from their connection to the precision medicine matrix.
Q4. What are some common misconceptions about precision medicine?
KY: A widespread misconception is that precision medicine is just about cancer genomics. We are addressing this by demonstrating that a multi-directional flow of information across basic, translational/clinical and population sciences germinates new questions, new insights, and new practices that strengthens all of these pillars of research.
The Marcus Program in Precision Medicine Innovation is proving this concept. The program funds collaborative team projects, grounded in a basic science question that extends into the clinical, population, or computational sciences. The remarkable research funded under this program and in similar partnerships demonstrates the potential and excitement of transdiscliplinary research that is fundamental to precision medicine.
Precision medicine is impacting research, health, and healthcare at UCSF, and those impacts are multiplying exponentially
Q5. A recent UCSF Magazine story* asked the question "Who Will Benefit From Precision Medicine?" What is your response?
KY: Everyone! First, precision medicine, as practiced here at UCSF, seeks to engage and acquire data across the full demographic, socioeconomic spectrum. Activities in our Precision Public Health and Precision Cancer Medicine programs (such as SF CAN) provide dramatic examples of those efforts. Second, the insights into disease that we gain through precision medicine research will reduce costs and increase efficacy of clinical trials and health care; they will also drive better prevention of disease. Success will translate into democratization of health and healthcare and movement toward health justice.
Q6. What else would you like everyone to understand about precision medicine?
KY: When we talk about aggregating and integrating all biological information, an understandable response is that this won’t happen for years or decades. In fact, a knowledge network doesn’t have to be finished to make a direct and positive impact. It’s not like assembling an airplane, which won’t fly safely until it’s complete. Bringing together increasing amounts and types of data, even if incomplete and in separate areas or programs, will still uncover novel insights and drive more informed decisions. Further iterations will then connect and merge those areas or programs.
Already, precision medicine is impacting research, health, and healthcare at UCSF, and those impacts are multiplying exponentially.

*"Who Will Benefit From Precision Medicine?" UCSF Magazine, Winter 2020